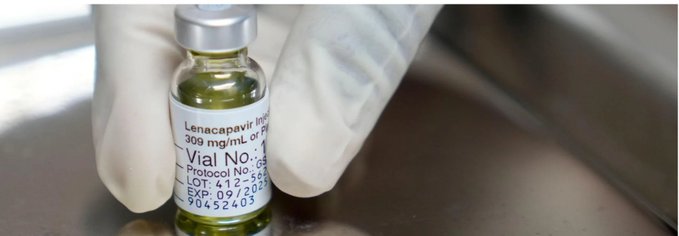
The U.S. Food and Drug Administration (FDA) has approved lenacapavir, marketed as Yeztugo, as the first and only twice-yearly injectable pre-exposure prophylaxis (PrEP) for HIV prevention—a milestone that experts are calling a transformative breakthrough in the global fight against HIV/AIDS. This approval, announced on June 18, 2025, marks a significant advancement in HIV prevention strategies, offering a new, long-acting option for individuals at risk of acquiring HIV.
How Lenacapavir Works and Its Clinical Impact
Lenacapavir is a first-in-class HIV-1 capsid inhibitor. Unlike daily oral PrEP regimens, which require strict adherence, lenacapavir is administered as a subcutaneous injection just twice a year, providing sustained protection against HIV. Its unique mechanism blocks the viral capsid, an essential protein shell, thereby preventing HIV from replicating in the body.
The PURPOSE 1 and PURPOSE 2 phase III clinical trials provided the foundation for FDA approval. These studies enrolled thousands of participants across diverse populations and geographies, including cisgender women in sub-Saharan Africa, cisgender men, transgender men and women, and gender non-binary individuals who have sex with partners assigned male at birth. The results were striking:
- 96% reduction in HIV incidence compared to background rates.
- ≥99.9% of participants receiving lenacapavir remained HIV negative throughout the studies.
Lenacapavir demonstrated superior efficacy to daily oral PrEP (such as Truvada), particularly in populations with challenges adhering to daily medication.
Addressing Adherence and Stigma
One of the most persistent challenges in HIV prevention has been medication adherence. Daily oral PrEP is highly effective—reducing the risk of sexual HIV transmission by about 99% when taken as prescribed—but real-world adherence is often suboptimal due to pill fatigue, stigma, and logistical barriers like regular pharmacy visits. Lenacapavir’s twice-yearly dosing removes the daily burden, making it a more feasible and appealing option for many, especially those in rural or resource-limited settings.
Experts emphasize that fewer healthcare visits and less frequent dosing could significantly increase PrEP uptake and persistence, particularly among populations disproportionately affected by HIV, such as young men who have sex with men, transgender individuals, and people in healthcare deserts. Dr. Carlos del Rio, a leading HIV researcher, noted that “a semiannual injection could effectively tackle significant challenges such as adherence and stigma that individuals on more frequent PrEP regimens often encounter”.
Safety and Side Effects
Clinical trials have shown lenacapavir to be well-tolerated, with the most common side effects being mild injection site reactions such as pain or swelling. No significant or new safety concerns were identified compared to existing PrEP options.
Global and Public Health Implications
The World Health Organization (WHO) has welcomed the FDA’s approval, highlighting lenacapavir’s potential to expand the HIV prevention toolkit and reach populations that struggle with daily or more frequent regimens. WHO plans to release guidelines for injectable lenacapavir during the International AIDS Conference in July 2025, aiming to support rapid and equitable access globally.
Lenacapavir joins a growing list of HIV prevention methods, including oral PrEP, the dapivirine vaginal ring, and long-acting injectable cabotegravir. Its discreet, long-acting formulation is expected to help overcome barriers such as stigma, discrimination, and inconsistent access to healthcare.
Access and Affordability Challenges
Despite its promise, access and affordability remain major concerns. The high price of lenacapavir could limit its availability, particularly in low- and middle-income countries, at a time when global HIV prevention funding faces cuts. Advocates and public health leaders stress the need for policy solutions to ensure that this breakthrough reaches those who need it most, not just those who can afford it.
Conclusion
The FDA’s approval of twice-yearly lenacapavir for HIV prevention is a historic milestone. By providing a highly effective, low-burden alternative to daily PrEP, it has the potential to transform HIV prevention efforts, bringing the world closer to the goal of ending the HIV epidemic. However, realizing this potential will depend on tackling the challenges of cost, access, and health system readiness—ensuring that this innovation benefits all communities at risk.

